Photobiomodulation Therapy
The science
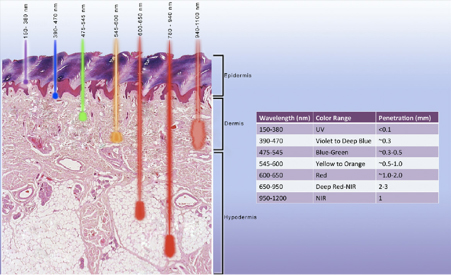
Red light and near-infrared wavelengths penetrate deepest into the head and body
Formerly known as Low-level Light Laser Therapy (LLLT), Photobiomodulation (PBM) Therapy is the application of light (usually a low power laser or LED) to promote tissue repair, reduce inflammation or induce analgesia.
Photobiomodulation Therapy has been the subject of several systematic reviews for a range of musculoskeletal pathologies with favourable conclusions reported by The Lancet [1], BMJ [2], International Association for the Study of Pain [3] and the World Health Organisation [4]. For numbered references referred to in the square brackets throughout this page click here.
Not a thermal therapy
Unlike other many treatments Photobiomodulation Therapy is a non-thermal therapy – it is more akin to photosynthesis. Photobiomodulation Therapy devices operate in the red and near-infrared spectra.
Sometimes pulsed and sometimes continuous beams are used. For acute and post-operative pathologies as little as one session is all that is necessary but for chronic pain and degenerative conditions as many as ten sessions may be necessary. Whilst other wavelengths have similar effects they do not penetrate nearly so well as the red and near-infrared range [5].
Applications
Arthropathies (diseases of the joints)
Degenerative disc disease
Fractures
Lymphoedema (abnormal collection of high-protein fluid just beneath the skin)
Myofascial pain (painful disorder that affects skeletal muscles in the body)
Neuropathies (problems with the peripheral nerves as opposed to the central nervous system)
Rehabilitation
Soft tissue injuries
Tendinopathies (diseases of the tendons)
Video introduction to Photobiomodulation Therapy
This 15 minute video starts with a 2 minute overview of Photobiomodulation Therapy (formerly known as Low Level Light Therapy) as it relates to THOR Photomedicine. United Nations Headquarters (New York) presentation to the Global Health Impact Forum on 6 May 2014 by co-founder James Carroll of THOR Photomedicine.
See LinkedIn article on James Carroll.
The Photobiomodulation Studio uses the company’s products because it believes that they are the best available.
Used with permission. © THOR Photomedicine
Mechanism of action (in laypersons’s terms)
The air we breathe and the food we eat is combined in the cell to create cellular energy called Adenosine Triphosphate (ATP). The actual processes that occur include the Kreb’s Cycle and the electron transport chain (ETC) which all occur within the mitochondria, the power plants of the cell. Located at the end of this ETC is an enzyme called Cytochrome C Oxidase (CcO). It is where oxygen attaches and ATP is produced with water as a by-product.
Now this really is in layperson’s terms
Want to know more about how food becomes energy but not quite sure about all this science stuff? You need this:
Reproduced with permission of the performers, Derrick Davis and Tom McFadden of Stanford University, California.
“If you have ever seen a metal object rust, you have seen oxidation. If left unchecked it can actually create holes in the metal.”
Cells in our body can undergo stress
However, when the cell(s) undergo stress, due to such things as cigarette smoking, too much sugar in our diet, too much sun on our skin, an injury etc, there will be an increased amount of free radical production. Specifically a molecule called Nitric Oxide (NO). This molecule has a higher affinity for that enzyme CcO than oxygen so it attaches there first.
There is then fewer or no place for oxygen to attach, so the cell is unable to produce as much ATP as it needs to function well and it becomes even more stressed, beginning to produce a very volatile free radical called Reactive Oxygen Species (ROS).
Typically the cell manages and neutralises ROS with rest and antioxidants, however the inability to do this fully results in oxidative stress. If you have ever seen a metal object rust, you have seen oxidation. If left unchecked it can actually create holes in the metal.
“When light of the correct colour and intensity is applied to the area of stress, the result is a return to the normal functioning of our cells.”
Oxidative stress is the underlying trigger for most diseases
In our cells, oxidative stress is accepted as the underlying trigger for most diseases and degenerative conditions. It is also a component in the inflammatory phase of acute and chronic injuries, as well as the ageing process.
However, when light of the correct colour, and intensity is applied to the area of stress, it immediately displaces the mNO from the receptor site CcO resulting in local vasodilation. This also allows oxygen to attach and begin the process of producing ATP. This removes the cause of ROS production, resulting in a reduction of oxidative stress and a return to normal functioning as our cells are programmed to do.
Stressed cells can benefit from light applied to them
Since every cell has hundreds to thousands of mitochondria, the primary receptor site for light, if light can be applied to the stressed ones with the correct colour and dose, those cells can benefit by a reduction in oxidative stress, increase circulation, increased ATP and the ability to begin normalising and healing.
Photobiomodulation Therapy is used successfully by sports clinics around the world
Mechanism of action (technical)
Most of the effects of Photobiomodulation Therapy can be explained by light absorption in the mitochondria [14-16]. Every cell in the body has lots of mitochondria (hundreds or thousands per cell). Mitochondria make cellular energy (ATP) from oxygen and pyruvate. In stressed or hypoxic (low oxygen) tissues, mitochondria make their own nitric oxide (NO) [17-19] which competes with oxygen. For numbered references referred to in the square brackets throughout this page click here.
The NO binds to Cytochrome c Oxidase (CcO) (the terminal enzyme in the electron transport chain) and displaces oxygen [20]. This displacement of oxygen has two negative effects; Reduced ATP synthesis Increased oxidative stress (leading to inflammation via the inflammatory ‘master switch’ NF-kB) [17-19, 21-23]. The effect of Photobiomodulation Therapy on hypoxic/stressed tissues can be described in several stages:
Primary effects
Absorption by Cytochrome c Oxidase (CcO) absorbs red and near infrared light
The transfer of light/photonic energy by this enzyme triggers a series of downstream effects [14, 24-26]. It is important to highlight how incredible this energy (actually packets of photons moving at 300 million metres per second) really is. The Northern Lights, aurora borealis, go some way in visually representing the wonder of it. The Lights are caused by charged particles from the sun hitting gases in the Earth’s atmosphere and interacting with the Earth’s magnetic field.
One of the secondary effects of Photobiomodulation Therapy is that damaged cells return to normal functionality
Secondary effects
Modulation of ATP, nitric oxide and reactive oxygen species
Changes in ATP, reactive oxygen species and nitric oxide follow light absorption by CcO. These effects are redox state and dose dependent. In hypoxic or otherwise stressed cells it has been shown many times that following Photobiomodulation Therapy, nitric oxide is released, ATP is increased and oxidative stress is reduced [27-31].
Tertiary effects
Downstream intracellular responses (gene transcription, and cellular signalling)
The downstream effects of Photobiomodulation Therapy released nitric oxide, increased ATP and reduced oxidative stress are many. They are context and cell type specific. Either directly or indirectly these biochemical intermediates affect components in the cytosol, cell membrane, and nucleus that control gene transcription and subsequently cell proliferation, migration, necrosis and inflammation [27-31].
Quaternary effects
Extracellular, indirect, distant effects
Tissues that have not absorbed photons can also be affected indirectly via secretions from cells that have absorbed light. Cells in blood and lymph can be activated and they travel significant distances from the session area to have distant (systemic) effects [32]. These can be autocrine, paracrine, and endocrine effects (sometimes known as a ‘bystander’ effects).
A clinical trial on football players with second degree ankle sprains found a significant reduction in swelling after Photobiomodulation Therapy
Oedema – lymphatic drainage
There is good evidence that Photobiomodulation Therapy also improves lymphatic flow. A systematic review of eight clinical trials of Photobiomodulation Therapy for post mastectomy lymphoedema concludes that, “There is moderate to strong evidence for the effectiveness of Photobiomodulation Therapy for the management of breast cancer related lymphedema” [33].
A controlled clinical trial on football players with second degree ankle sprains, found a significant reduction in oedema volume for the laser group compared with placebo laser (both groups also had rest, ice, compression and elevation) [34]. A laboratory trial on Carrageenan-induced oedema in the mouse paw found that treating lymph nodes alone was enough to reduce oedema in the mouse paw [35]. The mechanism of action is unknown.
Analgesia
Analgesic effects are probably via a different mechanism from the increased ATP/reduced oxidative stress model described above. According to a systematic review of laser analgesia mechanisms by Chow et al [36], higher power density laser light > 300 mW/cm2, when absorbed by nociceptors, have an inhibitory effect on Aδ and C pain fibres.
This high power density Photobiomodulation Therapy session slows conduction velocity, reduces amplitude of compound action potentials and suppresses neurogenic inflammation. Chow’s own laboratory studies show that Photobiomodulation Therapy blocks anterograde transport of ATP-rich mitochondria in dorsal root ganglion neurons. Varicosities result from this inhibition; this is normally associated with disruption of microtubules. This effect is completely reversible and lasts only 48 hours [37-39]. More work is needed to fully understand the complete mechanism of action.
Myofascial trigger points
Looking for the trigger point and therefore the best place to focus treatment on
Myofascial trigger points are palpable nodules in taut muscle bands and contraction of muscle fibres that lead to muscle spasms and limited joint movement. They are a component of several pain conditions, including migraine, tension-type headaches, temporomandibular disorder and neck pain.
The motor end plate is central to the aetiology of trigger points and EMG studies have shown abnormally high electrical activity over trigger points. Electrical activity is reduced after Photobiomodulation Therapy and clinical studies have shown that Photobiomodulation Therapy has immediate and cumulative effects on reducing pain [40-43], however the mechanism of action is not yet fully understood. For numbered references referred to in the square brackets throughout this page click here.
Protection against Parkinson’s and other neurodegenerative disorders with low-dose methylene blue and near-infrared light
Studies suggest that nerve cells (neurons) are metabolically protected against degeneration using low-level methylene blue and near-infrared light and therefore may help to prevent neurodegenerative disorders such as Parkinson’s, Alzheimer’s and Motor Neuron Disease.
The study at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4428125/ highlights these two very different, but beneficial, chemical-physical interventions and the exciting future for therapeutic applications.
Research
To date more than 400 randomized double blind placebo controlled clinical trials have been published with some professional guidelines suggesting Photobiomodulation Therapy is used as part of standard care.
This includes:
World Health Organisation (WHO) Task Force on Neck Pain systematic review [4]
The Lancet Systematic review of LLLT for Neck Pain [1]
International Association for the Study of Pain (IASP) fact sheets for Myofascial Pain Syndrome, osteoarthritis and neck pain [3]
British Medical Journal (BMJ) Systematic review and guidelines for treating tennis elbow [2]
American Physical Therapy Association (APTA) Systematic review and clinical practice guidelines for achilles tendinopathy [8]
British Journal of Sports Medicine (BJSM) Systematic review for frozen shoulder [7] European Society for Medical Oncology (ESMO) Clinical practice guidelines for oral mucositis [9]
Multinational Association for Supportive Cancer Care (MASCC), Clinical practice guidelines for oral mucositis [10]
For numbered references referred to in the square brackets above click here
Research articles
Effects of low-power light therapy on wound healing: LASER x LED
Biostimulation effects of low-power laser in the repair process